In the late 1980s, many ceramic supply houses sold chemicals without warning labels, but I had been careful when working with them, especially with MnO2 (manganese dioxide) or related materials. I always wore gloves and a dust filter mask and worked mostly outdoors. However, I did not realize that even when firing in the open air the vapors escaping the kiln contained volatilized materials from my glazes, and a simple dust filter would not protect me. I blamed my violent nausea after each raku firing on carbon monoxide and tried to avoid inhaling any smoke.
Even though I was aware that manganese is considered a highly toxic material, it took me a long time to realize that my becoming ill might have anything to do with my raku pottery work. There were no sudden indications or changes. My health slowly got worse and worse, but I kept finding excuses. I told myself that I was still recovering from post-surgical complications of a spinal fusion and was also under great emotional stress: good enough reasons to feel miserable. It is impossible to be objective when one is in pain.
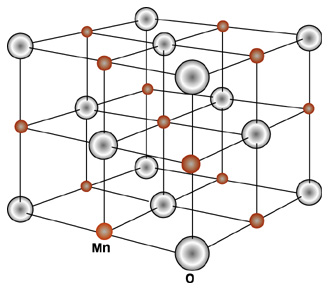
Manganese, a metal ore, is omnipresent on earth. It exists, in various concentrations, in rock, soil, on the ocean floor and, often because of pollution, in water and in the air. It is mined throughout the world, mostly for use in steel production, but it is found in such everyday things as the common dry-cell battery, fertilizers, fuel additives, welding rods, incandescent light bulbs, magnets, certain bronzes, etc. Its ores and the chemicals made from them are used as coloring agents for bricks, glass and ceramic products, as well as dyes, paints and varnishes. It is contained in fungicides and pharmaceuticals. Many minerals, including carbonates, oxides, silicates and borates contain manganese. It is also added to animal and poultry feeds.
Potters have found manganese useful not only as a glaze colorant (yielding hues ranging from brown to pink and purple) at all temperatures but as a body colorant and surface colorant, either as a key ingredient in a slip or used alone. Above 1090°C manganese is an active flux; applied by itself on top of a clay body it sinters, developing surfaces ranging from a slight luster to a bronze sheen. It has been a favorite of clay sculptors for years because a thin wash of manganese dioxide and water will color the clay body without destroying surface texture. In fact, if the wash has been applied to bisqueware, allowed to dry slightly then wiped repeatedly with a damp sponge, relief areas are accentuated. Contemporary “bronze” glazes, which no doubt have their origin in the work of the late Lucie Rie, rely on a relationship of manganese to copper with varying additions of other ingredients. For a more complete discussion of manganese and its applications to ceramics, readers may wish to refer to sources such as The Potter’s Complete Dictionary of Materials and Techniques by Frank and Janet Hamer or The Illustrated Dictionary of Practical Pottery by Robert Fournier.
Manganese is an essential trace nutrient for microorganisms, plants and animals, including all mammals and birds. It is present in most foods, particularly in whole grains, cereals and some nuts such as pecans, Brazil nuts and almonds. It is abundant in black pepper, cloves, ground ginger, thyme, bay leaves and especially in tea leaves, whereas most meats, fish and dairy products contain smaller trace amounts.
With a well-balanced diet, humans are not likely to suffer from manganese deficiency.
Medical reports of neurologic disorders associated with manganese date back to the mid-19th century. Overexposure and resulting manganese intoxication seem to be concurrent with the Industrial Revolution and thus job related, i.e., predominantly found in manganese miners and steel production workers. The Second World War’s demands for increased steel production resulted in an increase in documented cases of manganese poisoning. (There is also an instance of discarded batteries polluting well water and affecting a fairly large group of people in the immediate environment.)
There is little doubt in my mind that I am alive today and relatively healthy because of my admiration for Hans Coper and because of my love for his pottery. I had never met him, yet I mourned his death in 1981 as I might have mourned the death of a friend. He died, at the age of sixty, of pneumonia, but he had been suffering from another illness for many years. If I had not bought Tony Birks’ book Hans Coper to learn more about the artist, I probably never would have read the following passage:
Hans was now undergoing tests in connection with his increasing difficulty with speaking, walking and using his left hand. Motor-neuron disease, or amyotrophic lateral sclerosis (ALS) was diagnosed in 1975. His doctor explained to him as much as was known of this illness. The degeneration of motor-neurons in the cortex of the brain, and their fiber tracts, produces a slowly developing paralysis. There is no known cause and no cure.
News of his illness filtered through to all those connected with ceramics, and it was widely rumored that Hans was suffering from manganese poisoning, an occupational hazard for those who worked with the element. In Hans’ case this was a plausible assumption, since manganese dioxide was the one metal oxide that Hans used constantly. It is important for other potters who spend much time with the material to know that Hans’ illness had nothing to do with manganese, or with any other metals, and that it is very unlikely that there is any connection between pottery making and ALS (emphasis mine).
Eventually, I compiled the notes I had made of my symptoms:
Within a few days of firing, I got severe headaches, nausea, which got worse over the next three months, accompanied by a great fatigue, sleep disturbances: insomnia; inertia, disinterest in friends and environment, in my own work. Confusion, losing things, forgetting things, dizzy-giddy feeling. Feeling of unreality, episodes of “white-outs”, not knowing where I was or what I was doing, losing things during those periods. Even losing whole hours of time. No energy. Changes in handwriting: illegible even to myself. Vision getting worse, even though nothing organically wrong; esp. left eye, feels swollen, seems to have gravel on it, extremely sensitive to light. Finding it more and more difficult to follow oral or written instructions; complete loss of three-dimensional perception and visualization. Unable to do subtraction in math. Forgetting words, even very simple descriptive ones. Unable to finish sentences, my tongue seems paralyzed. Make mistakes all the time, forgetting foreign languages I learned recently. Dropping things, spilling things, stumbling over my own feet, cramps in legs at night, reflexes slowed down, can’t drive car. Feels like short-circuit from head to hand. Occasional problem with bladder control. Absolute disinterest in sex. Terrible headaches mostly unilateral left side. Doing madly impulsive things; very restless, irritable. Making awful social blunders and faux-pas. I’m just not me any more! Lost my energy, my creativity, my sense of humor, motor skills, and am losing my mind from the headache. Physio (cranial-sacral therapy) provides temporary relief, at first up to several days, now about two hours. Wake at night because of severe headaches. Relief through icepacks temporary. Heat, fatigue, stress, driving aggravate.
These were changes in my life-long patterns of feeling and behavior. Other people might be affected differently or not as severely.
Hhen I saw them all together, I recalled what Tony Birks had written about Hans Coper’s illness, particularly the passage about his use of manganese. I can’t help being skeptical and suspicious of all categorical statements. Since I had been using manganese dioxide for at least twenty years–although in very small amounts (about two teaspoons per firing a couple of times a year)–at times even scraping it out of dry-cell batteries, I thought I might have myself tested for MnO2 poisoning.
With my mixed bag of symptoms, and afraid of being labeled a hypochondriac, I made the round of doctors, beginning with a family physician. He could not really help me, but he agreed to my request to have myself tested for MnO2 . It was not easy to find a laboratory in 1987 that would check for manganese. My blood sample had to be sent to Laval, Quebec. Test results confirmed that I was suffering from chronic MnO2 toxicity (my results showed 98 nmols per liter; normal is 10 to 20). This test was done six months after my most recent exposure. It is quite likely that immediately after the raku firing the toxicity level was much higher. (As I discovered later, manganese intoxication cannot be accurately diagnosed through laboratory tests unless they are done quite soon after exposure. Later diagnosis often has to rely on neurobehavioral testing.)
In the meantime, a psychiatrist looked at my list of symptoms, asked what kind of work I was doing and said that I did not need him but a neurologist. The first neurologist I consulted suggested I had either multiple sclerosis or a brain tumor. I was very lucky to be then sent to Tee Guidotti, physician, and Head of the Occupational Health Program at the University of Alberta in Edmonton. He confirmed the diagnosis of MnO2 poisoning, and added that though he was very good at diagnosing, he was not so good at treating this particular disease.
I went through a two-day battery of neuro-psychological testing. It consisted of tests for general intelligence, learning and memory, language and communication, basic mathematics, reading capability, verbal fluency, response speed, manual dexterity, etc. It showed short-term memory loss, slowed-down reflexes, problems storing information, and I can’t remember what else. Not until late 1990 did I finally have access to a magnetic resonance imaging (MRI) scan. The MRI scan provides visual evidence of cerebral deposits of paramagnetic metals. Test results were “inconclusive”: “The left basal ganglia demonstrates a mild reduction in signal intensity on all sequences. Decreased signal intensity in the left basal ganglia of questionable significance. The possibility of some metal deposition cannot be excluded.”
I began a rather withdrawn life. Panic attacks hit me whenever I had to drive, follow instructions, do more than one or two things at a time, or was faced with making any decisions. My mind simply shut down. I could only function, day by day, in a very familiar environment, only felt “safe” at home. I could no longer work with clay or wood or anything else I loved to do.
The instinctive initial reaction on being diagnosed was to write it all down and try to get it published somewhere to make sure this never happened to anybody else. But I was unable to motivate myself enough to sit down to write. Most of the time, I could literally not put two sentences together.
The years between 1987 and 1992 are essentially lost. There is hardly anything I remember. One day recently, I came across a copy of the November/December 1991 issue of Equinox. It published a rather lengthy article by Alec Ross on toxic metal threats, including MnO2 and its suspected connection with Parkinson’s disease. Ross quotes John Donaldson, former associate professor of pharmacology at the University of Manitoba and an authority on manganese poisoning, as saying that manganese sets off a destructive chain reaction in the brain, that is “like an atomic bomb going off in the cells.” The article goes on:
Donaldson first began uncovering the toxic powers of manganese in the mid-1970s while searching for the causes of Parkinson’s disease. A degenerative illness that usually occurs late in life, Parkinson’s disease is characterized by an increasing rigidity of the muscles and by palsied movement. Although previous research had shown that the disease appears when the level of an essential chemical known as dopamine plummets in the brain, the origins of the illness remained a mystery.
While browsing though the scientific literature in search of a clue, Donaldson noticed a strange connection to manganese. Twenty years earlier, in the 1950s, American researcher George Cotzias reported that Chilean miners exposed to large quantities of manganese-laden dust developed long-term clinical symptoms resembling those of Parkinson’s disease. And on the Pacific island of Guam, natives who mined the local manganese deposits suffered a startlingly high incidence of both Parkinson’s disease and a form of dementia associated with amyotrophic lateral sclerosis, or Lou Gehrig’s disease … Donaldson wondered whether the presence of manganese in the brain could precipitate the decline in dopamine (emphasis mine).
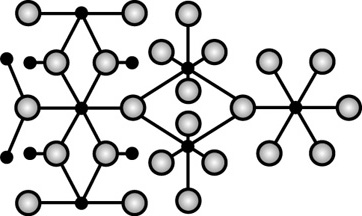
Donaldson’s further experiments “suggested that manganese would wreak the greatest havoc in areas of the brain where the biochemical conditions were alkaline. As it turned out, such conditions existed in the basal ganglia, the region of the greatest cellular damage in Parkinson’s disease patients.” Donaldson eventually found that manganese and dopamine react and release small quantities of hydrogen peroxide. This reaction released a free radical that could destroy tissues “as surely as if they’d been irradiated.”
Moreover, the destructive particle could also break down a key part of the brain cell’s defense system. In other words, the presence of manganese could evidently trigger a complex sequence of neurochemical reactions that attacked not only the structure of the nerve cell but also the system by which it could defend itself. Recalled Donaldson: “We got a double whammy from manganese.”
Another curious effect of manganese seems to be its connection with violent behavior. According to Ross, the most interruptive inmates in California prisons have been found to have “significantly higher levels of manganese in their hair samples than do less troublesome inmates.” And the connection between manganese and “mayhem” has been known s since the 1700s, when it was observed that “the aboriginal inhabitants of Groote Island, a tiny island off the northern coast of Australia, were considerably more warlike and hostile than their neighbors. Today, the island is home to the world’s largest manganese mine.”
At the time this article appeared in Equinox, Donna Mergler, who was then a researcher at the University of Quêbec at Montréal, was collecting information on the early neurotoxic effects of manganese exposure among smelter workers in a ferromanganese and silicomanganese production plant. The results were published in Environmental Research in 1994. The findings “are consistent with current knowledge on brain Mn activity and suggest that manifestations of early manganism can be observed in well designed population studies, using sensitive (neurofunctional) testing methods.”
In April 1990, The Nova Scotia College of Art and Design hosted a symposium on Health and Safety in the Arts. Trying to get more information on manganese intoxication, I contacted Rosemary Marchant, one of the physicians who made presentations at the symposium. She was at that time at the Faculty of Medicine of Dalhousie University. Marchant informed me that results of a study in Sweden were to be published in the Scandinavian Journal of Work Environment and Health, in 1991. This was to be “a study of a small number of workers exposed to Mn, not complaining of any problems but demonstrating subtle neurological changes when exposed to levels below the recommended TLVs [Threshold Limit Values].”
In her letter, she goes on to say: “As the usual effects of MnO2 exposure are on the nervous system and sometimes the lungs, the specialists most likely to help you would be neurologists and respirologists, if there was available treatment.” She said that there are “only a tiny number of individuals in Canada with an interest in health and the arts,” so she suggested Michael McCann, Industrial Hygienist and Executive Director, Center for Safety in the Arts, New York City, as a resource person. The Center, which suspended operations in July of 1996, published a newsletter and an extensive list of books, pamphlets and articles, as well as videotapes on hazards in the arts. (While this issue was originally being researched, I could obtain no help from the Center.)
Encouraged recently by Tee Guidotti to learn more about manganese toxicity, I looked up the 1991 Scandinavian Journal research report Rosemary Marchant had referred to. It confirmed that the effects of low-level exposure “were interpreted as early (subclinical) signs of disturbances of the same type as Parkinsonism.” The Swedish study summarized its findings:
Our results show that long-term exposure to very low levels of manganese in the air may interfere with the normal functioning of the central nervous system. These effects are interpreted as a preclinical stage of the full-blown manganism previously reported from high-level occupational manganese exposures.
A later study (1993), which was based on the Neurobehavioral Core Test Battery of the World Health Organization, confirmed that
of the thirty-seven symptoms related to the nervous system, twenty were more frequently reported by the exposed workers. (They) had significantly poorer motor speed, visual scanning, visuomotor coordination, visuomotor and response speed, and visuomotor coordination and steadiness. A clinical examination did not reveal any abnormality among the two groups. (Patients and referents). Hence a neurobehavioral test battery may be a more sensitive method than a clinical examination in detecting early changes in motor function among manganese-exposed workers.
That same year, a five-year follow-up study (C.C. Huang, “Progression after chronic manganese exposure,” Neurology, August 1993) of patients with chronic manganese-induced Parkinsonism who had been removed from manganese exposure found that “patients with manganese-induced Parkinsonism may develop increasing neurologic dysfunction long after cessation of exposure and that their responses to levadopa [a drug for treatment of Parkinson’s disease] are different from those of patients with Parkinson’s disease.”
I have quoted from these medical journals in some detail because there is so little published anywhere, and not many physicians have the information readily available to them. It is really up to artists to observe changes in their behavior or health patterns, just as it is their responsibility to exercise proper precautions when working with potentially harmful materials.
There is no treatment for the effects of excessive and dangerous amounts of manganese absorbed by inhalation. If working with the material, one must prevent exposure through the use of proper protection (a properly fitting mask with the appropriate filter). Potters exposed to fumes given off during glaze firings at all temperatures are at the greatest potential risk and need to keep informed on how to protect themselves. If an unsafe amount is inhaled, either through dust or volatilized vapors emitted during firing, the body will eventually excrete the toxin via the gastro-intestinal tract and the bile, but the damage it might have caused cannot be undone.
I can’t resist including a bit of prehistorical manganese trivia. Some 7000 years ago, for about a period of 2000 years, an ancient pre-Inca fishing tribe living on the coast of today’s Chile and Peru, the Chinchorro, preserved all their dead through the sacred rite of mummification. (See “Chile’s Chinchorro Mummies,” National Geographic, March 1995.) This was done about 2000 years before the Egyptians developed their particular embalming techniques. The Chinchorro used a fairly elaborate procedure which involved taking apart and then rebuilding the body into a human form. For potters, it might be interesting to learn that, as a “glorious final touch,” they covered the body with a coat of black manganese paint. This paint, after it had dried to a dull finish, “was buffed to a high sheen with a smooth piece of wood or possibly a wave-worn pebble.” They literally burnished their dead! This particular “black period” of mummification was abandoned about 2800 b.c. in favor of red ochre paint. Nobody really knows why. Did they run out of manganese? Did red become a favored color? Or did they know more than we do about what has often been called “manganese madness?”
I was hesitant at first when it was suggested I consider writing about my personal experience with manganese toxicity. There was my lack of medical knowledge, there was the fear of living through it all over again, but curiosity and the initial concerns I had to inform other potters of the hazards of raku firings won out. In a way, putting it all on paper became a very cathartic experience. I have really gotten it out of my system now. I contacted Tee Guidotti, the physician who originally diagnosed my case; he kindly agreed to discuss my preliminary notes and to answer questions:
TG: I am not going to comment on the mechanism of manganese, because it is too technical and there are too many unknowns, although the mechanism you are describing in the article certainly makes a lot of sense.
EB: What do you mean by mechanism? The way I got poisoned?
TG: No, the way that manganese actually damages the basal ganglia and induces Parkinson’s disease. I don’t think we know for sure, and I would not venture an opinion on the molecular level, but we certainly do know that there is substantial disruption of an area called the substantia nigra and the elaboration of dopamine in parts of the brain that controls movement, and this causes Parkinson’s disease.
Actually, at one time there was a popular theory that maybe manganese exposure, or some extraordinary problem with manganese metabolism, was responsible for community cases of Parkinson’s disease, or at least a minority of cases of Parkinson’s. I don’t think that theory is particularly subscribed to any longer, but it is a reflection of just how perfectly manganese can reproduce Parkinson’s disease. There is no feature of Parkinson’s that manganese toxicity cannot mimic, so a lot of people think that it is the same disease.
The cases of overt manganese toxicity that I have personally seen, other than yours and maybe one or two others, were all in China, and they have all been associated with welding of ferromanganese alloy. This alloy is very popular in railroads, because unlike others, the more stress it receives, the stronger it gets. But the people who weld it, particularly people who have minimal protection, are at very high risk. I have seen a metallurgist who had developed the disease and any number of railroad workers.
There are other descriptions in the literature of manganese toxicity that are not so clear-cut. And these nonParkinsonian neurotoxic cases seemed to resemble your own case a bit more. There the picture was dominated more by what we call the soft signs in Parkinson’s: cognitive function changes, emotional lability, short-term memory deficits, that kind of thing, rather than the tremor and the gait abnormality that is so common in overt Parkinson’s. I think that it may very well have to do with how the exposure took place, because the Parkinson’s picture seems to be more a function of frequent, repeated exposures that may not be as dramatic as yours at the time. In your case you have probably, in retrospect, had astronomical exposures.
Now your syndrome is probably very complicated, as well, because you probably had a second problem going on at the same time: metal fume fever.
EB: Metal fume fever from the manganese or also any other metals?
TG: Probably from the manganese, but from other metals as well.Light metals like copper, manganese, cadmium, magnesium, if volatilized and inhaled all at once in concentrations, will get into the blood, get into the body, but the concentrations are not necessarily high enough to get into the brain and cause neurotoxicity. However, you can produce an illness that looks for all the world like a bad case of flu. Typically, it is over in a couple days, but you feel absolutely miserable while it is going on.
EB: I did use a lot of copper, some iron and cobalt.
TG: Cobalt has other toxic properties and can be very dangerous itself; iron not so much. Copper can very much produce metal fume fever [which] only lasts a period of time and then goes away by itself. In metal fume fever, compared to neurotoxicity, although the concentration of metal inhaled is very high, the total amount of metal inhaled is not that great because it is limited in time. It is a little bit like the difference between being drowned and being knocked over by a wave.
The high concentration just does not persist in the body, and that is why metal fume fever is not the same thing as metal neurotoxicity. But I suspect that what you had was metal fume fever occurring repeatedly after the firings and then, in addition, you were doing that often enough, in high enough concentrations, so that over a period of time you accumulated the manganese, and that it was responsible for many of the neurotoxic syndromes you had.
Now, way back in 1987, we did not have available the trace element analysis laboratory that we do today, and I think it would be very interesting to repeat the manganese level. It would not necessarily change anything involving treatment that we’d recommend.
EB: Would I not have eliminated the manganese by now?
TG: Yes, you probably would. It could well be normal by now.
EB: I think Laval retested me about a year ago and it came back normal.
TG: Their laboratory technology is very close to what we have here. In fact, the person who runs the Laval laboratory has been out to visit here. One of the reasons was that the two laboratories use similar technology; they compare notes. So if you had a test from Laval, it is probably okay.
The main difference here is, and the reason I would very much have liked to have had this test available in 1987 in your case, is that instead of just looking at a single metal or a small group of related metals, this one test does fifteen all at once, so you get quite a profile. I suspect that you were higher in a number of light metals, not just manganese, but that the toxicity picture was dominated by manganese.
That basically was all that I was going to say. If you’d like some historical material on manganese, I’ve got an excellent book [Manganese] that was published in 1973 by the US National Academy of Sciences. Clearly, with the date, it has become a little bit obsolete in terms of research, but the historical material is still quite sound.
EB: I have a few questions. Obviously, the first one is, who should get tested? Would you recommend anybody working with raku pottery be checked?
TG: Personally, I am impressed with the hazards of raku. I think that as beautiful as it is, and it is gorgeous. I have many pieces – the raku firing technique potentially can be quite dangerous. It would not be a bad idea for people using raku to get tested, preferably fairly soon after the firings, [to] get a picture of how much they are exposed.
This recommendation has to be tempered a little bit by reality. The most accurate trace element analysis tests are not readily available. We can do them here, and the material can be sent to our laboratory and to Laval, but commercial laboratories don’t do this test the same way. It is not that they are sloppy, but the test itself may not be as accurate. At these levels accuracy really counts. [Ceramists wishing to be tested] should try to get plugged into a trace element analysis laboratory that is associated with a major university or medical center. They should not get sucked into other operations because they will be very disappointed and the results will be uninterpretable. Quite frankly, the symptoms that can be attributed to manganese can also be very much confused with an anxiety state. It’s tricky. Some people feel anxious, depressed, nervous about things completely aside from any possibility of manganese toxicity. People who have nonmanganese related disorders [could receive] an inaccurate manganese reading, put two and two together and get five, and that is not good. It is not good medicine, and it gives a very false picture of their own personal problems.
So, faced with that, I think that yes, I believe that people should be screened, but they should only be screened by people who know what they are doing.
I would hate to have people misconstrue this whole thing and to create a false epidemic of suspected manganese toxicity. At the same time, I personally believe that there are probably a lot more cases out there because of the high exposure opportunities.
EB: What do I do to avoid exposure, what kind of filter cartridges would you recommend, is there is anything at all that would work?
TG: Well, the big one, of course, is ventilation.
EB: I worked outdoors and it did not do any good.
TG: But you were probably also subject to whichever way the wind was blowing. There is also personal protection – masks and such. Go to an industrial safety supply store, and talk to the representative. There is a big chart and, depending on what you are working on, this chart tells you which cartridge works for which exposure situation.
EB: Would it be under vapors or metal fumes?
TG: The metal fume cartridge would be the one to use for working around firing kilns. [Potters] doing dry work with high silica-containing clay or something like that should use the dust cartridge. It’s a good idea to discuss with the representatives in some detail the specifics of how you are using materials.
EB: Is manganese in any form toxic, or is exposure to vapor worse than inhaling dust, for example?
TG: Vapor appears to be worse than dust. Manganese content in dust, in clay and that sort of thing is not necessarily bio-available; so, although it is true that many clays and many other minerals contain manganese, that manganese is not necessarily available for distribution in the body once it is inhaled. As a practical matter, the biggest problem is the fumes.
EB: Is there a safe exposure level?
TG: You want to keep your exposure to the absolute minimum. That means not taking a target like an occupational exposure level and giving yourself a false sense of security because you are below that level. Be well below that to ensure that any slip-up or failure in your system does not push you over the line. Fortunately, manganese is not quite so much a problem as lead. Lead is a problem because you can ingest it in so many different ways, and because it tends to be more bio-available. In the case of manganese, you don’t have to worry about foods and that sort of thing.
EB: If one is found positive, as happened to me, what do you recommend that people do? Would chelation therapy, for example, right after exposure be of any use?
TG: No, in fact, chelation therapy can be dangerous. There are problems with chelation and calcium metabolism, particularly in the case of women who are prone to osteoporosis and low calcium. You want to be sure you are not draining your body of calcium content. Likewise, the complex of some metals and the chelating agent can be very dangerous to the kidneys. So that’s also a problem. The chelating agents are quite toxic themselves intrinsically.
EB: It has been suggested to me to consider that kind of treatment.
TG: I think that would be a mistake. Whatever damage that has been done has been done. And I think that the chelation would only add another layer of confusion because it would essentially add another chemical exposure.
Remember we are not talking about a heavy metal here. We are talking about a light metal, and light metals tend to be handled by the body differently. Chelation therapy tends to be most useful for things like lead and arsenic, and even there we have to be very, very careful because of the toxicity of chelation. But it is not useful at all for manganese.
EB: What about recovery and treatment. There really is not much, is there?
TG: Well, for the Parkinsonian cases, we actually know a great deal, and stand to learn even more thanks to the Chinese. For the kind of shadow cases, the borderlines, which I think your case fell into, we don’t know enough about thm. We haven’t followed them long enough to know what the natural history is.
EB: I have been, and still am, getting physiotherapy treatment. It seems to have helped with all aspects of the disease. Acupuncture combined with cranial-sacral and other techniques. There was really nothing else that anybody could do, and it seemed to loosen my muscles, help my headaches and vision, everything else.
TG: I think, again, that for these atypical cases symptomatic treatment is the answer. You have, in your case, the muscle control issues that were addressed directly by physiotherapy, and so on.
People with overt Parkinson’s disease have particular therapy options, L-dopa, for example, or Methadopa, but there is no suggestion that it would be particularly helpful in the atypical cases. So, I think when you have a classical Parkinson’s that is related to manganese of the kind I was seeing in China, the treatment is highly specific. The treatment for the atypical case, such as yours, is more focused on whatever symptoms are troubling the patient and dealing with them one at a time.
Manganese has been treated as a sort of medical curiosity, and you won’t find very many books about it, for example, because it has not been perceived as a common problem. It has been perceived as a sort of an oddball.
The University of Alberta Extension Department, Edmonton, is hosting an International Symposium in May 1996. Tee Guidotti was invited to give a talk on ceramics and health hazards at that time.
Elke Blodgett is a potter in Edmonton, Alberta. See “A Very Personal Statement,” the article she wrote about her work, in the Winter 1994/95 issue of Contact.